32nd Annual Magic City Sports Medicine Conference
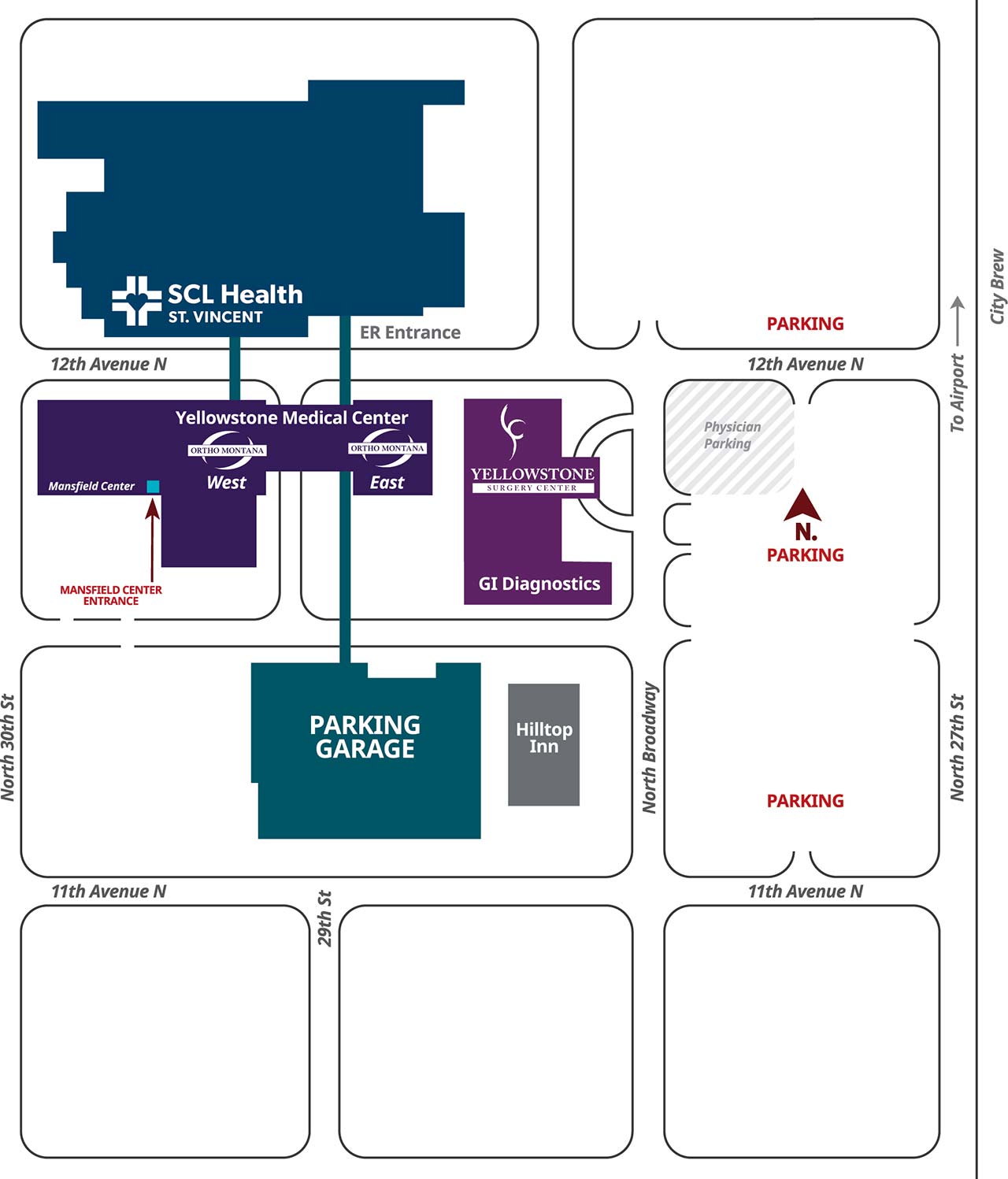
Saturday, May 20, 2023 | 7:30AM – 5:30PM | Mansfield Health Education Center | Billings, MT
Date: May 20th, 2023
Conference Theme: Contact Sports
Presenters: Tyler Clark-MD, Jim Elliott-MD, Laura Opstedal-DPT, Steve Klepps-MD, Eric Neal-MD, Josh Bowler-MD, Justin Smith-CSCS, Ben Phipps-MD, Heather Hansen-MD, Anna Kasperick-RD, Lauren Hasquet-DPT and Dayne Dyer, CSCS
Domains:
I: Injury and Illness Prevention and Wellness Promotion
II: Examination, Assessment and Diagnosis
III: Immediate and Emergency Care
IV: Therapeutic Intervention
V: Healthcare Administration and Professional Responsibility
Objectives: Following this program attendees will be able to:
- Identify the special anatomical considerations for the skeletally immature patient, including the unique features of pediatric bone
- Classify pediatric growth plate fractures according to the Salter Harris Classification
- Explain General principles for pediatric fractures and dislocations
- List common injuries extremity fractures and dislocations
Participant Assessment: A quiz will be given to assess learning as well as all attendees must complete a program assessment and evaluation. Upon completion of these a Statement of attendance will be issued.
From the BOC Approved Provider handbook: Professional practice gap is the difference between the current state of “what is” and the desireable or achievable state “what should be” in regards to competency, performance and/or patient outcomes. Educational need is defined as the need for education on a specific topic identified by a gap in professional practice. This is the foundation of developing compliant CE programs under BOC requirements.
The goal of any CE activity is to change competence and/or performance and’or patient outcomes.
Professional Practice Gap: The 32nd Annual Magic City Sports Medicine Conference is an annual sports medicine conference that focuses on the education of athletic trainers, physical therapists and other allied health care fields. At the conclusion of the 31st Annual Magic City Sports Medicine Conference, an evaluation from the attendees was collected and those results were tabulated. The results from the evaluations requested specific topics to be discussed by the Orthopedic surgeons such as shoulder instability, fracture management and specific return to play criteria.. The results also requested for updates and advancements in the field of orthopedics.
Educational Need: The planning committee for the 32nd Annual Magic City Sports Medicine Conference identified topics and speakers to meet the practice gap and educational needs.
The focus of this year’s conference is on “Contact Sports” in sports medicine. The Athletic Medicine and Performance (AMP) team of orthopedic surgeons, physical therapists, athletic trainers, registered dieticians and strength and conditioning personnel will work towards the same goal of returning an athlete back to their specific sport regardless of the type of injury.
The term athletes cover the full age spectrum and an allied healthcare professionals (PTs, ATs, RDs, CSCS, LMTs, etc) must be able to treat these athletes who do not fit the model traditionally taught in school. Health care professionals (HCP) should know general principles for pediatric and adult injuries including evaluation, pain management, splinting/casting guidelines, and compartment syndrome. HCP should be able to apply this knowledge to practice in assessing and managing of injuries including fractures, instability, nonoperative versus operative and referral process.
HCP should also be culturally competent/sensitive. The difference in treatment strategies from one geographic region to another varies. The anatomy and physiology are constant, but treatment standards vary dependant on resources, practitioner knowledge and cultural standards.
Clinical Bottom Line:
Athletic trainers, physical therapists and other allied health care professionals need to be cognizant of the differential diagnoses for injuries in order to be able to identify, refer, treat and return to play for each specific case. An interdisciplinary team cohesively networks to improve the outcome of patient care as these professionals work together to accurately diagnose, treat – including surgical interventions and rehabilitate and recondition patients to return to activity/sport. Treatment plans, appropriate referral strategies, understanding of surgical techniques, nutrition services and prevention and reconditioning programs are all key components to individualized plans of care.
References: will be on presentation slides
PowerPoint/Google Slides will be available for all attendees on the AMP website: www.ampmontana.com
Speakers will disclose any conflicts of interest during their presentation and abide by Copyright law (see www.copyright.gov).
Educational Gap for: Title: Emotional Intelligence and Why it is Important for Sports Medicine Providers
Athletic Trainers (ATs) frequently find themselves working in highly emotional situations. These situations range from telling coaches that their star players are done for the season to helping athletes cope with the loss of their identity when they are no longer able to participate. Emotions run high on and off the sports field or court. ATs must be able to perceive, manage, and understand emotions as well as utilize emotions to guide thoughts and actions. In other words, ATs must possess emotional intelligence (EI) which Salovey and Mayer (1990) in their groundbreaking work defined as “the ability to monitor one’s own and others’ feelings and emotions, to discriminate among them and to use this information to guide one’s thinking and actions” (p. 189).While other healthcare fields have researched the impact of EI, the issue has not been adequately researched in the athletic training context. EI is a necessary part of the skills, knowledge, and abilities of ATs. According to McCloughen and Foster, “EI is a key component of effective leadership, a mediator of the stress response, an influential component of inter-disciplinary teamwork and potential remedy for deficient communication” (2018, p. 2705). Yet without sufficient research regarding EI in athletic training, it remains unknown as to what level of Emotional Intelligence Athletic Trainers tend to possess and what, if any, correlation exist between EI and the experience, age, and biological sex of ATs (Jessen, 2017).In addition to patient outcomes, high EI benefits the healthcare providers directly. EI is related to the ability to communicate as well as the ability to manage stress. Some studies have even shown an inverse relationship between EI and burnout. Despite the importance of EI in healthcare, there is no published research regarding EI in athletic training, a field that deals directly with emotions on a daily basis. By assessing the EI of experienced athletic trainers and comparing it with that of students entering the profession, patterns can be identified. Previous studies indicated individuals can develop and improve their EI.
References for above:
Jessen, J. L. (2017). Lived Experiences and Insight on Development of Emotional Intelligence in Professional Nursing Practice. College of Saint Mary.
McCloughen, A., & Foster, K. (2018). Nursing and Pharmacy Students Use of Emotionally Intelligent Behaviours to Manage Challenging Interpersonal Situations with Staff During Clinical Placement: A Qualitative Study. Journal of Clinical Nursing, 27, 2699-2709.
Salovey, P., & Mayer, J. D. (1990). Emotional Intelligence. Imagination, Cognition and Personality, 9(3), 185-211.
Learning Objectives:
- Following this presentation, attendees will be able to list the four branches of Emotional Intelligence (EI).
- Following this presentation, attendees will be able to explain the importance of EI within sports medicine.
- Following this presentation, attendees will be able to assess EI using the Schutte Self Report Emotional Intelligence Test (SSEIT).
NSCA Credits: Pending Approval.